
Hospital-based AMS interventions 1–3, 16, 17 and digital interventions supporting AMS 18–20 have been the focus of previous reviews. 15 These issues can hamper uptake of systems and so reduce effectiveness of digital interventions in practice. For example, implementing too many CDS alerts can lead to alert fatigue, 14 many stand-alone systems do not interface with existing clinical information systems, and digital interventions are not always user-friendly. 13 Despite these benefits, research has also identified a range of challenges and risks associated with the use of AMS digital interventions. For example, an alert signalling de-escalation to narrower-spectrum agents can assist prescribers in making appropriate antimicrobial choices at the point of prescribing. Integrating restriction policies and implementing guidelines can also be done more efficiently with the use of CPOE 10–12 and clinical decision support (CDS). 10 These can be overcome with computerized provider order entry (CPOE) systems or electronic medical records (eMRs), which allow an AMS team to easily identify patients on an antimicrobial and enter notes into the system to document and communicate recommendations to prescribers.

For example, difficulty identifying patients receiving suboptimal therapy and difficulty communicating recommendations to prescribers were barriers to undertaking audit and feedback. Many AMS programme barriers previously cited in the literature can potentially be addressed with the use of digital interventions. 7–9 AMS processes that were traditionally paper-based are gradually becoming computerized with the increasing implementation of information technology in hospitals.

The use of digital interventions within AMS programmes is recommended by international guidelines.
4 AMS programmes have been shown to reduce inappropriate antimicrobial use, hospital length of stay, costs, rates of resistance and hospital-acquired infections. mortality and length of stay) and readmission rates have been used by studies to assess the impact of AMS in hospitals. 2, 3 A range of outcome measures including antimicrobial use, cost, resistance patterns, secondary infections, patient outcomes (e.g. 1 A plethora of studies have been published evaluating the impact of different AMS programmes and interventions on antimicrobial prescribing and patient outcomes. 1 AMS programmes are typically hospital-wide and multifaceted, including strategies such as prescribing guidelines, formularies and approval systems, post-prescription audit and feedback, and point-of-care interventions. Meets or Exceeds Standards for ANSI 250.4 and ANSI 250.Antimicrobial stewardship (AMS) is a term used to describe programmes aimed at optimizing antimicrobial use, ultimately improving patient outcomes, and reducing adverse consequences including antimicrobial resistance, in a cost-effective way. It is recommended that finish paint (top coat) be applied after installationġ61 (cylindrical lock), 86 Edge (mortise lock), Deadbolt, RPD (blank edge, panic reinforced)Ĭontinuous Hinge Application (Undersized Width), Exit Device Trim, Lite and Louver Cutouts Heavy Gauge Door Closer and Hinge Reinforcementsġ4-Gauge Inverted Top and Bottom Channels, Optional Flush Top Capįactory-Applied, Baked-On, Rust Inhibiting Gray Primer (No Special Color Options) – Not intended to be a finish coat.
AMS TIMELY DOOR FRAMES FULL
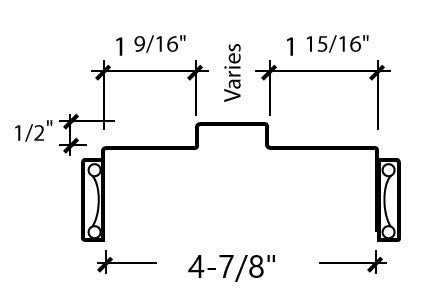
Square Hinge and Lock Edges (Beveled Edges Available) – Full Height, Epoxy Filled Mechanical Interlock Edges Standard Widths up to 4'0", Height to 8'0" (Custom Sizes Available) Non-Handed Design Reversible Hinge Plates Heavy Duty, SDI Level 2 – 18-Gauge Steel Face Sheets – (16 Ga.


 0 kommentar(er)
0 kommentar(er)
